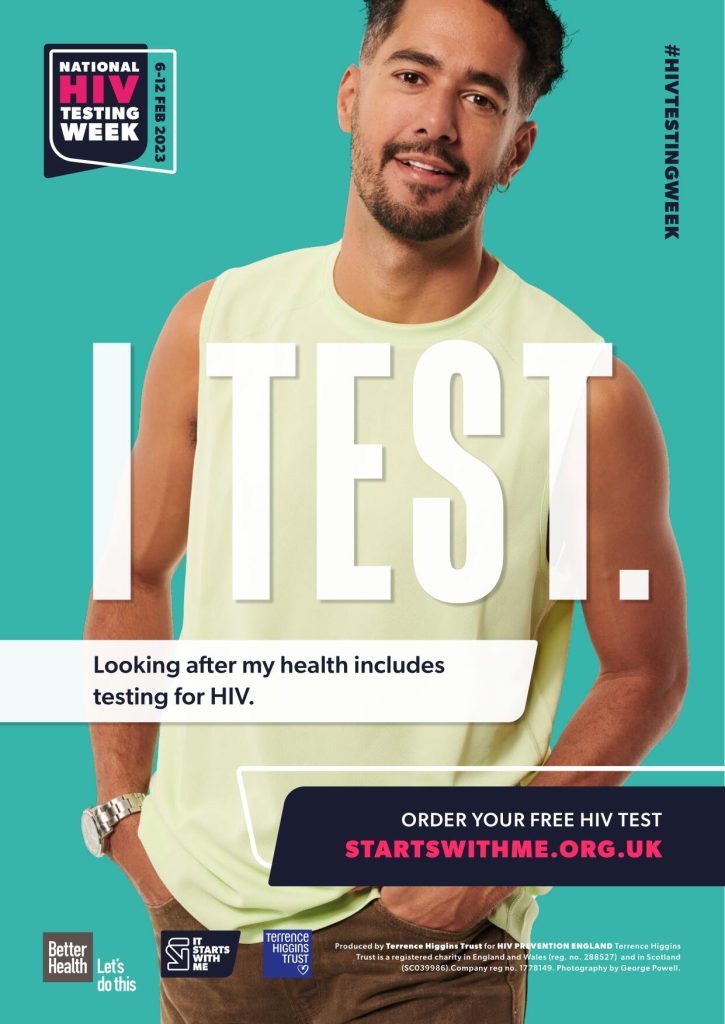
The It Starts With Me summer campaign focuses on raising awareness of why and how to prevent sexually transmitted infections (STIs) including HIV. To find how you can support this exciting campaign download and read our Get Ready for a Hot Summer campaign briefing [PDF].
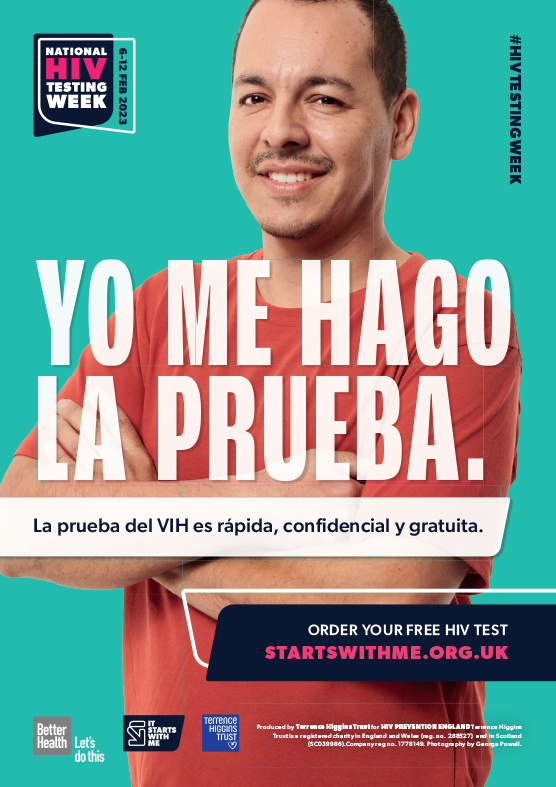
The campaign, using the tagline ‘Get ready for a hot summer’, is delivered through digital platforms and face to face outreach. The target audiences for the campaign are:
- gay, bisexual and other men who have sex with men (GBMSM)
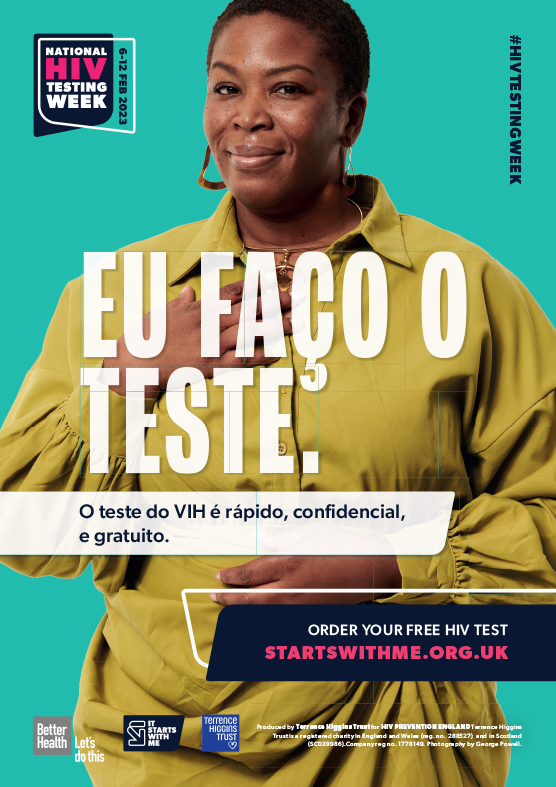
- heterosexuals of Black African ethnicity
- people from other communities affected by HIV.
Key messages for this campaign:
- As you get ready for summer, it is important to protect yourself from HIV and STIs.
- Your sex life should be pleasurable and healthy, find out how to look after your sexual health this summer.
- Sex without a condom increases your likelihood of getting an STI.
- You could have an STI without knowing it.
- PrEP is a pill that can prevent you from getting HIV.
How can you get involved?
Free resources
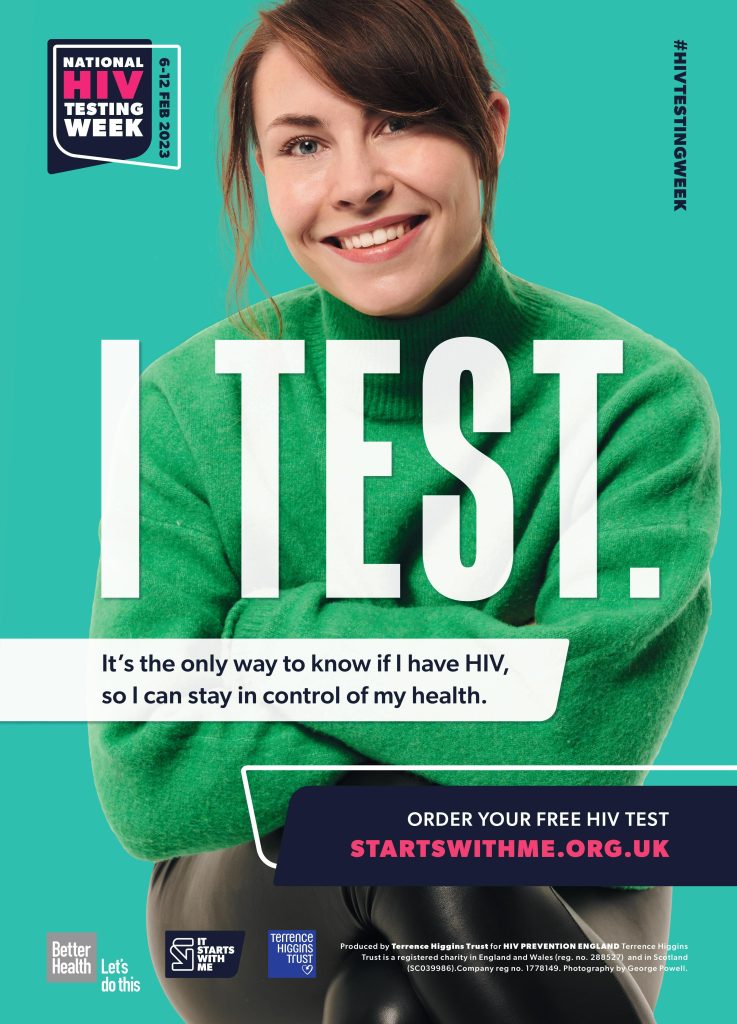
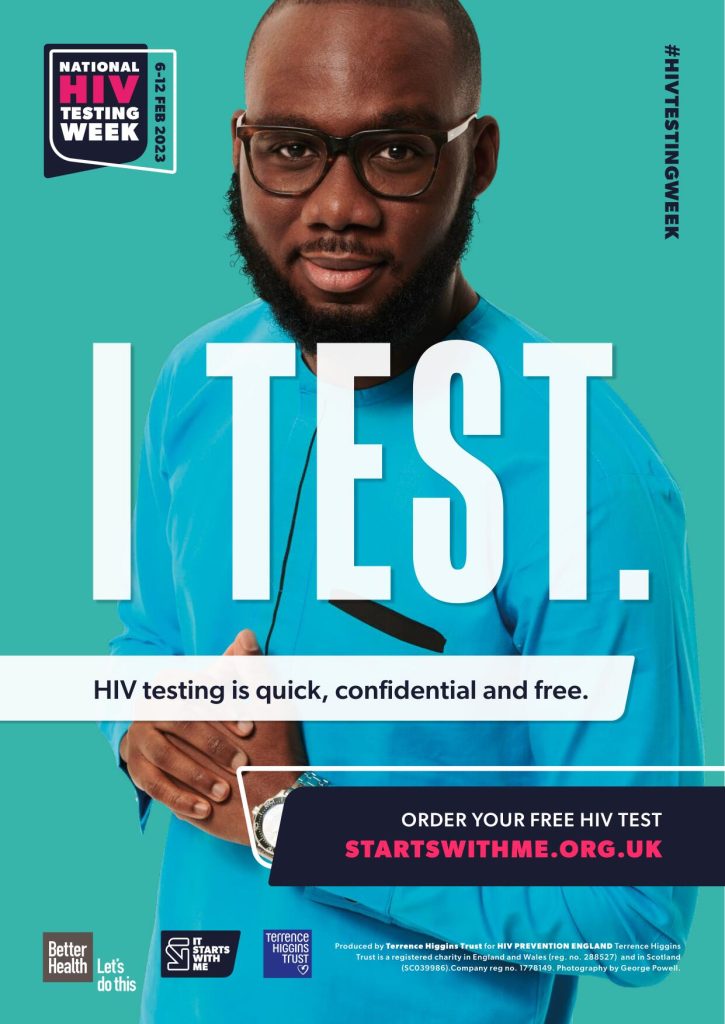
Our resources portal is now open with new posters, leaflets and merchandise for outreach, health promotion activities and raising awareness of HIV and STIs in your clinic, GP surgery, organisation or community.
New resources for summer 2023:
- ‘The facts about PrEP’ leaflet
- Get ready for a hot summer, STI, condom and PrEP posters
- Summer-themed merchandise.
Social Media Pack
The social media pack is now available to download. It includes a selection of correctly sized images for use on Facebook, Twitter, Instagram (including Instagram stories) or any other social networks, as well as some suggested messaging.