Written by Renaissance UK
PrEP is a word that anyone working within the sexual health sphere will be very accustomed to, and despite its only recent NHS availability the popularity of this game changer has skyrocketed. However, there are many communities (particularly those at risk) who have not yet heard of PrEP and its benefits.
So how to make people aware?
Renaissance UK, a sexual health and harm reduction charity based in Lancashire, picked up the mantle of this question and ran with it. There are many answers to this problem, some cheap, some expensive – but all had the same fundamental flaw: they were out of our control. Once the money had been spent, the charity would be left hoping for the best in terms of engagement and response.
However, for every problem, there is a solution. Enter Patricia, The Little Sexy Bus.

Patricia is an ex-events vehicle which has been repurposed to provide a clean, clinical, educational space for anyone who wants to know about HIV prevention and ultimately, PrEP.
No expense has been spared in making Patricia: warm, inviting and of course, accessible. Renaissance have created an interior complete with consultation space, television, hot and cold water, air conditioning and an awning for those really sunny days.
Every available space on the inside and outside of the van has been given over to promotion. This means that even those who may not feel comfortable coming to talk might at least get a taste of what is on offer and can investigate in their own time. The sides of the van all have QR codes which link directly to the campaign’s website: bepreped.co.uk.
However, the greatest advantage of Patricia is her mobility. Static advertising works for many campaigns, particularly when your target audience is the public at large. However, when you want to reach specific groups thinking outside the box is the way forward. This is what Patricia brings to the table. She can go to places that other traditional advertising cannot reach, and doubles up as a space where we can test and have confidential conversations.
During National HIV Testing Week, we launched Patricia with a tour across Lancashire. We visited Lancaster and Morecambe in the north, Skelmersdale in the south, Burnley in the east and many, many more places in between. Not only was this an opportunity to test and raise awareness about PrEP but surprisingly it also served as a chance to challenge some of the misconceptions about HIV.

Looking to the future, Renaissance UK is going to seek out opportunities to work collaboratively with other organisations in the area including charities, NHS groups and sexual health services. This collaborative approach to health promotion and support is mutually beneficial to all involved and shows what can be achieved with some joined up thinking.
Patricia will also be making an appearance at all of the local Pride events, providing a platform with which we can do outreach, testing and provide advice all from the comfort of a cosy consultation space.
Like Patricia’s (The Little Sexy Bus) name suggests our intention is worn on our sleeves. We intend to facilitate positive and constructive conversations about HIV and sexual health. We are about unapologetically promoting safer sexual health practices and destigmatising at every opportunity. That coupled with Patricia’s mobility means we can take the messages to where they need hearing most.
We are extremely proud and look forward to Patricia’s impact on PrEP promotion around Lancashire.
See you on the road.


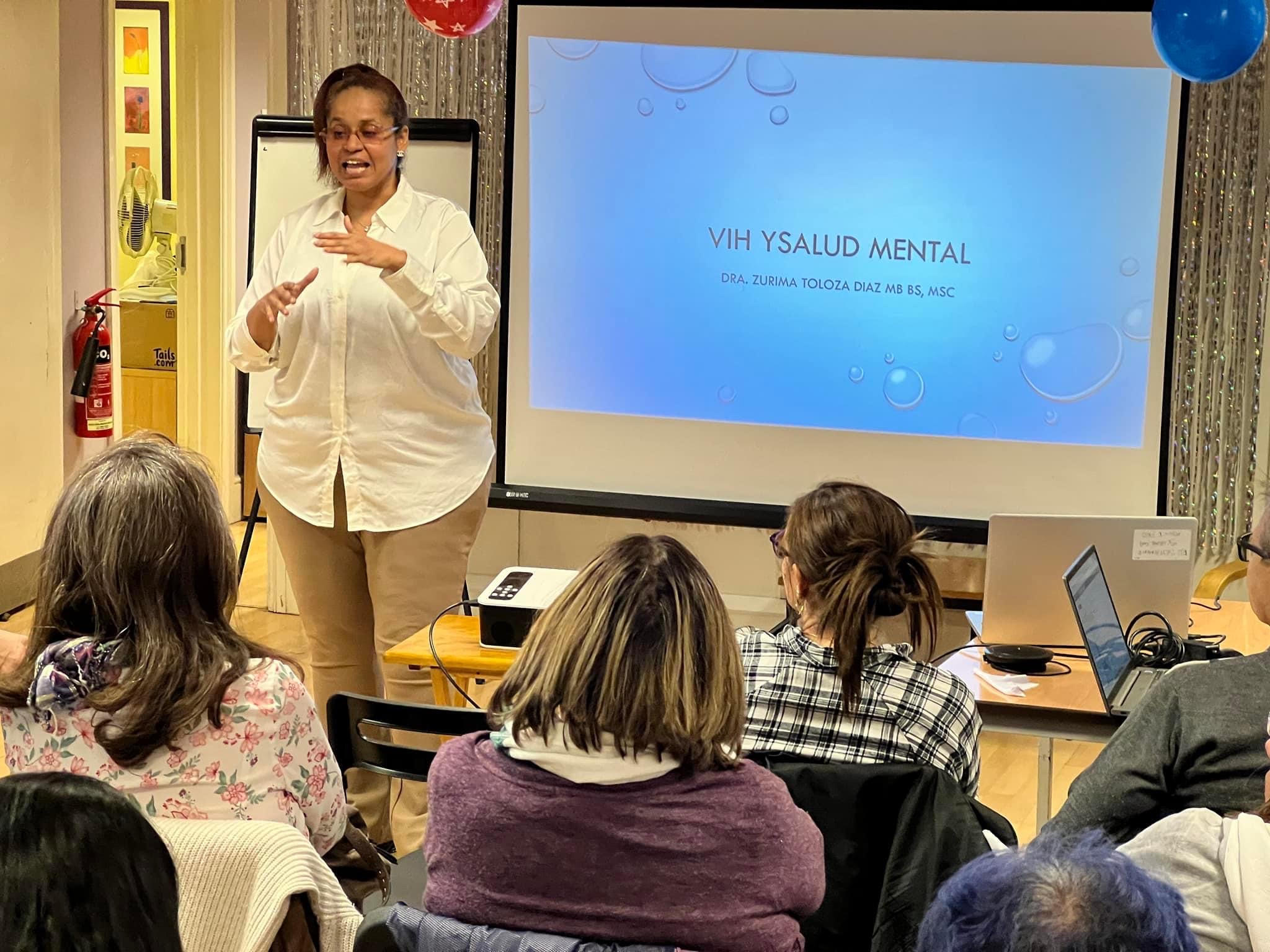 Zurima kindly shared her contact details with some attendants to book appointments with her. For community members who do not speak fluent English, and have mental health concerns, receiving insights and advice from an expert in their own language is a great experience. The evaluation of the session was performed by asking every attendee what they took with them from the session, how useful the information provided was, and what they will now do differently. After the workshop, there was a space for social dialogue and an opportunity to ask Zurima and Carlos any questions.
Zurima kindly shared her contact details with some attendants to book appointments with her. For community members who do not speak fluent English, and have mental health concerns, receiving insights and advice from an expert in their own language is a great experience. The evaluation of the session was performed by asking every attendee what they took with them from the session, how useful the information provided was, and what they will now do differently. After the workshop, there was a space for social dialogue and an opportunity to ask Zurima and Carlos any questions.