In May, Public Health England (PHE) published their Hepatitis C in England 2020 [PDF] report. In order to improve national surveillance of the cascade of care for the first time, PHE included data on people attending sexual health services and people who are homeless.
Of the estimated 89,000 people in England who are chronically infected with hepatitis C (HCV), many are from marginalised and underserved groups in society. It is hoped the new and updated data will help to identify where improvements can be introduced to stop people falling through the net.
Co-infection in people living with HIV can be common in certain population groups. The liver has an essential role in processing medicines used to treat HIV and other conditions. Viral infections that affect the liver, such as hepatitis A, hepatitis B and hepatitis C, can make the liver less able to process medicines properly. This is one of the reasons the British HIV Association (BHIVA) have introduced targets for the micro-elimination of HCV in people with HIV.
Testing in sexual health services (SHS)
- The number of individuals tested for HCV in sexual health services shows an increase of 37.4% between 2014 and 2018.
- The proportion of individuals testing anti-HCV positive (reactive or positive antibody test means you have been infected with the hepatitis C virus at some point in time) shows little change over the same time period, remaining at around 1.3% (1.2 to 1.4%).
GUMCAD data (from 2014 to 2018)
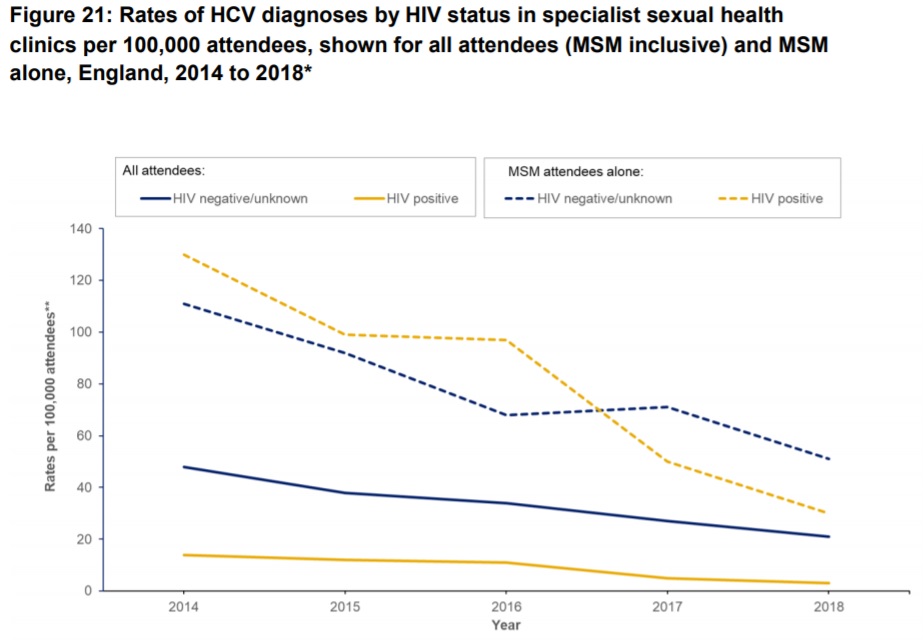
- Decrease in rates of HCV diagnoses in all individuals attending specialist SHSs in England.
- Among attendees of negative or unknown HIV status, rates decreased from 48 per 100,000 attendees to 21 per 100,000 attendees (fall of 56.3%).
- Among HIV-positive attendees, the decrease was greater from 14 to 3 per 100,000 over the same period (fall of 78.6%)/
- The lower rates are attributed to people living with HIV (PLWH) being diagnosed with HCV in their HIV care rather than in SHS.
- Compared to the overall rate in all attendees, men who have sex with men (MSM) showed elevated rates of HCV diagnoses regardless of HIV status: likely due to high-risk behaviours including higher number of condomless anal sex partners, and injecting recreational drug use.
HIV/HCV co-infection
BHIVA has targets for the micro-elimination of HCV in people with HIV: curing HCV in 80% of those co-infected by April 2019, 90% by April 2020, and 100% by April 2021.
HARS data suggests that of people with HIV accessing care in England:
- 0.69% (598/86,997) tested positive for either an acute or chronic HCV infection in 2017
- 1.47% (1,298/88,002) in 2018
In 2018 HCV prevalence highest in:
- People living with HIV who inject drugs (27%)
- MSM living with HIV who inject drugs (6.5%)
Lowest in:
- Heterosexual men living with HIV (0.8%)
- Women (0.5%)

Impact and opportunities of COVID-19
While the COVID-19 pandemic poses a threat to HCV elimination targets, it has also presented opportunities to test and link individuals from some underserved groups into care.
Many local authorities and charities worked together during lockdown to support homeless people and rough sleepers by moving them off the streets into individual hotel rooms. This provided a unique, short-lived opportunity to reach out to this group to address some health needs while their accommodation was more secure.
In June The Martin Fisher Foundation and EmERGE M-Health Ltd launched a new partnership to provide Hepatitis and HIV testing in Brighton and Hove for approximately 200 temporarily housed rough sleepers in the city.
Working with outreach workers from Brighton & Sussex University Hospitals NHS Trust and the Terrence Higgins Trust, aided by St Mungo’s support workers, colleagues visited hotels to offer screening using a simple finger-prick test. All face-to-face interactions involved the use of personal protective equipment (PPE). The project incentivised people to test by offering them £5 food vouchers for their engagement.
107 people had been tested through the programme by 20 July 2020. Processing lab results takes some time but from the cohort of the first 25 individuals tested, five HCV infections had been identified, which is broadly in line with the anticipated HCV prevalence. There were no HIV diagnoses within the first 25 tests returned.
Normalising testing and enabling early access to treatment, which reduces onwards transmission risk of both viruses, has the potential to significantly reduce the public health impact of HIV and HCV during the next decade.
A combined method of upscaling integrated testing and exploring innovative ways to reach people most likely to be affected by HIV/HCV co-infection (as we have seen during the COVID-19 epidemic) would help to achieve this.
