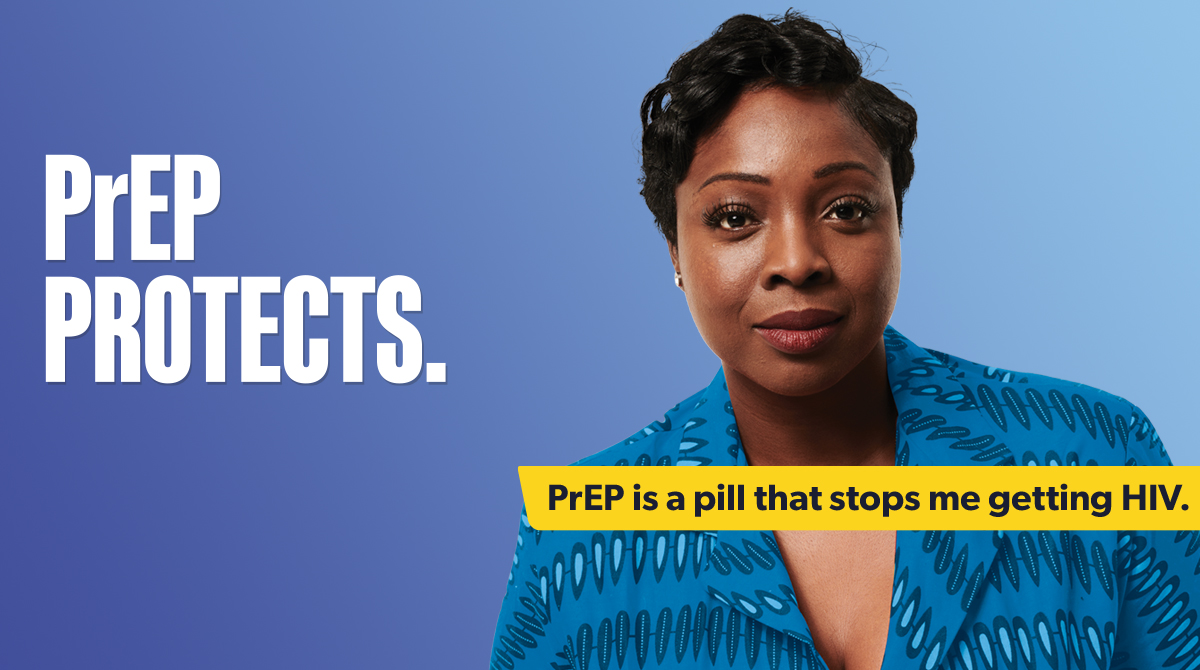
The summer 2025 phase of the It Starts With Me campaign focuses on raising awareness of PrEP as a method for HIV prevention.
The campaign, using the tagline ‘PrEP Protects’, will be delivered through digital platforms and face-to-face outreach. It will run from July to September 2025.
The target audiences for the campaign are:
- gay, bisexual and other men who have sex with men (GBMSM)
- heterosexuals of Black African ethnicity
- people from other communities affected by HIV.
Why do we need this campaign?
Reducing the likelihood of people getting HIV remains a key public health priority across England. PrEP is a highly effective drug that if taken before being exposed HIV can prevent HIV acquisition.
However, data from UKHSA’s latest report on PrEP in England show that inequalities in accessing PrEP continue to exist by gender identity, sexual orientation, and ethnicity.
Among GBMSM, the data indicate:
- a 7% increase in HIV diagnoses first made in England between 2022 and 2023.
- the highest increase in new diagnoses is among GBMSM of Black African ethnicity
- PrEP need was highest among GBMSM (70%)
- GBMSM of Black ethnicity were least likely to have their PrEP need identified and least likely to initiate or continue PrEP.
The PrEP Protects campaign will respond to the trends in the data by raising awareness of PrEP among GBMSM, in particular how to access it and provide information on the different dosing options. Particular attention will be given to reaching GBMSM of Black ethnicity and others who are not aware of or have not considered reasons that PrEP’s might be relevant to them.
Among heterosexual men and heterosexual and bisexual women, the data indicate:
- HIV diagnoses first made in England rose by 36% and 30% among men and women respectively between 2022 and 2023
- PrEP need was less likely to be identified among heterosexual men and women (61% and 62% respectively), compared with GBMSM (85%)
- PrEP need was least likely to be identified among heterosexual people of Black ethnicity.
The data trends show there is a need to raise awareness and knowledge of PrEP among heterosexual men and women, in particular, those of Black African ethnicity.
Campaign activities
The campaign features an informative creative, prompting people to learn more about PrEP and find out whether this is an HIV prevention tool for them.
The campaign will:
- provide information on what PrEP is, where people can get PrEP, and how to take it
- direct people to an online journey, which will take users to different pages depending on their existing knowledge of PrEP
- raise awareness of PrEP through outreach at summer events across England
The campaign will be promoted via digital platforms and social media, face-to-face outreach, press coverage, and through influencer engagement.
Get involved